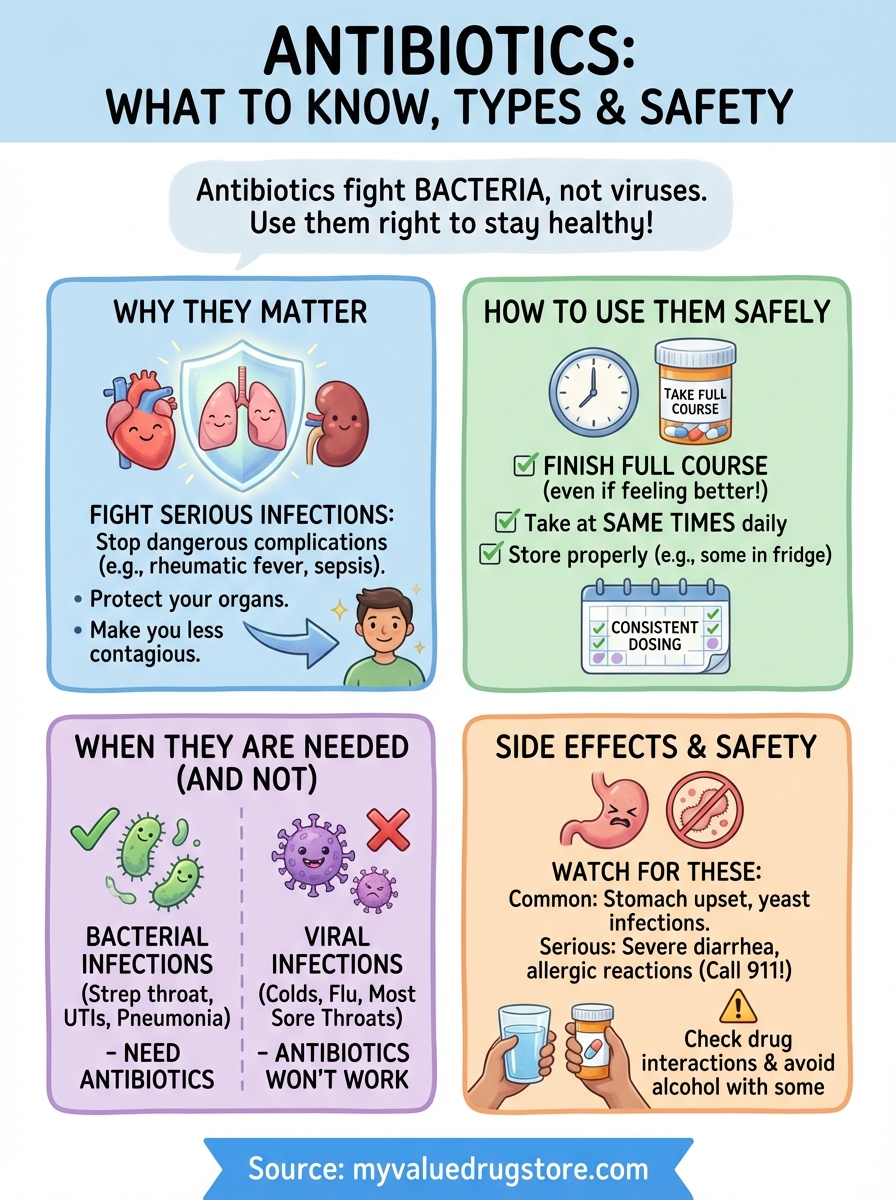
Antibiotics are medications that fight bacterial infections by killing bacteria or stopping them from multiplying. Your doctor prescribes them when harmful bacteria cause illnesses like strep throat, urinary tract infections or certain skin infections. These medications save lives and prevent serious complications, but they only work against bacteria. They can’t treat viral infections like colds, flu or most coughs.
This guide breaks down what you need to know about using antibiotics safely and effectively. You’ll learn when antibiotics are necessary, which infections they treat, and how to take them properly to get better faster. We’ll cover the most common types your doctor might prescribe, potential side effects to watch for, and why finishing your full prescription matters. You’ll also discover when antibiotics won’t help and what alternatives might work better. Understanding these basics helps you make informed decisions about your health and get the most benefit from your treatment.
Why antibiotics matter for infections
Bacterial infections can turn from manageable to life-threatening without proper treatment. Antibiotics for infections work fast to stop harmful bacteria from multiplying in your body, giving your immune system the support it needs to fight back. Your body naturally fights off many infections, but some bacterial invaders multiply faster than your immune defenses can handle. When bacteria overwhelm your system, you need antibiotics to regain control and prevent permanent damage to your organs, tissues or overall health.
They prevent serious complications
Untreated bacterial infections spread beyond their starting point and create dangerous complications. A simple urinary tract infection can travel to your kidneys and cause permanent damage or sepsis, a life-threatening condition where infection spreads through your bloodstream. Strep throat left untreated can lead to rheumatic fever, which damages your heart valves, or trigger kidney inflammation. Skin infections like cellulitis can penetrate deeper tissue layers, enter your bloodstream, and require hospitalization. Antibiotics stop these infections before they escalate, protecting your organs and potentially saving your life.
Taking antibiotics as prescribed stops bacteria from causing permanent damage to your body.
They protect others from spreading bacteria
Some bacterial infections spread easily from person to person through coughing, touching, or close contact. Taking antibiotics reduces the amount of bacteria in your body, making you less contagious to family members, coworkers, and others around you. Strep throat becomes non-contagious within 24 hours of starting antibiotic treatment, allowing you to return to work or school safely. Whooping cough requires antibiotics to prevent transmission to vulnerable people like infants and elderly individuals who face serious health risks from infection. Your treatment protects both your recovery and the health of your community.
How to use antibiotics the right way
Following your doctor’s instructions exactly determines whether antibiotics for infections work effectively in your body. Many people make mistakes that reduce how well these medications work or create dangerous bacteria that resist treatment. Your prescription label tells you the dose, timing, and duration of treatment tailored to your specific infection and health status. Taking antibiotics correctly helps you recover faster, prevents the infection from returning, and protects you from developing resistant bacteria that no longer respond to treatment.
Take the full course even when you feel better
You’ll likely feel better within a few days of starting antibiotics, but stopping early allows surviving bacteria to multiply and potentially develop resistance to the medication. Your symptoms disappear before the medication eliminates all harmful bacteria from your body. Finishing your prescription ensures you kill every last bacterium causing your infection, preventing a relapse that might require stronger antibiotics or hospitalization. Throw away any leftover antibiotics after completing your course, and never save them for future illnesses or share them with family members who seem sick.

Follow the timing and dosage instructions
Taking your antibiotics at consistent intervals maintains the right amount of medication in your bloodstream to fight bacteria effectively. Missing doses or taking them at random times creates gaps that allow bacteria to recover and multiply between treatments. Set phone reminders or pair your doses with daily routines like meals or brushing your teeth to stay on schedule. Some antibiotics work best on an empty stomach, while others require food to prevent stomach upset or improve absorption. Read your prescription label carefully and ask your pharmacist if anything seems unclear about when or how to take your medication.
Consistent timing and proper dosing keep antibiotics working effectively in your system to eliminate infection.
Store and handle antibiotics properly
Improper storage destroys the chemical structure of antibiotics and makes them ineffective at fighting your infection. Keep most antibiotics at room temperature in a cool, dry place away from direct sunlight, heat sources, and moisture. Bathrooms seem convenient but create too much humidity that damages medications. Liquid antibiotics often require refrigeration after opening, so check your label or ask your pharmacist about storage requirements. Never flush unused antibiotics down the toilet or throw them in regular trash where children or pets might find them. Take leftover medications to a pharmacy take-back program or follow FDA disposal guidelines to protect your family and environment.
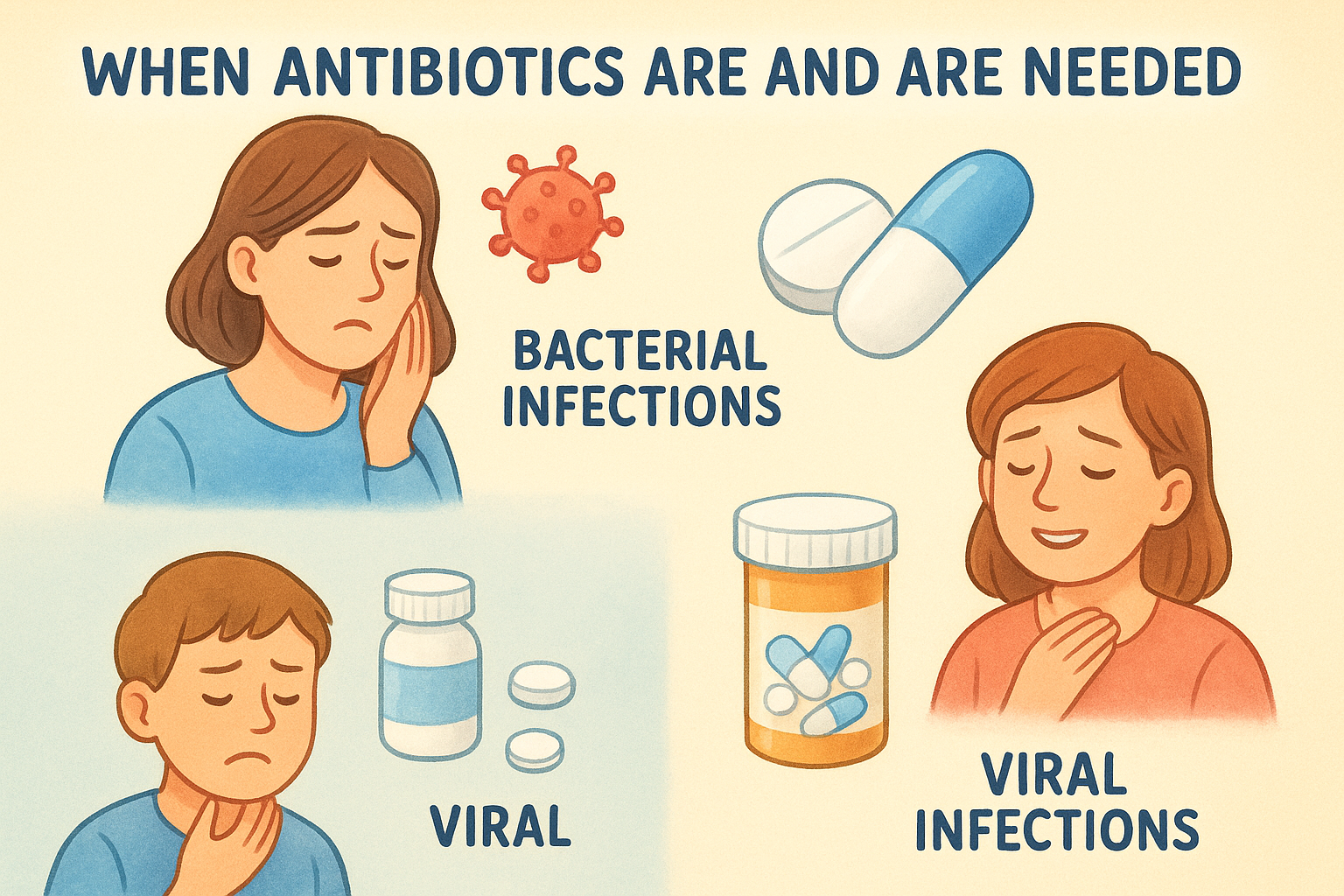
When antibiotics are and are not needed
Understanding when you need antibiotics saves you from unnecessary side effects and helps preserve these medications’ effectiveness for future infections. Doctors prescribe antibiotics based on the type of infection you have, not simply because you feel sick or miserable. Bacterial infections require antibiotics, while viral infections and some mild bacterial infections heal on their own with rest and supportive care. Taking antibiotics when you don’t need them exposes you to side effects without any benefit and contributes to antibiotic resistance, making these lifesaving medications less effective when you truly need them.
Bacterial infections that require antibiotics
You need antibiotics for infections caused by bacteria that your immune system can’t clear on its own or that could spread to others. Strep throat requires antibiotics because untreated infection can damage your heart valves or kidneys, and you remain contagious to others without treatment. Urinary tract infections need antibiotics to prevent bacteria from traveling to your kidneys and causing permanent damage. Bacterial pneumonia, whooping cough, and serious skin infections like cellulitis also require antibiotic treatment to prevent life-threatening complications. Your doctor runs tests like throat cultures or urinalysis to confirm bacterial infection before prescribing antibiotics, ensuring you receive the right treatment for your condition.
Antibiotics only work against bacterial infections, not viruses, so proper diagnosis matters for effective treatment.
Viral infections where antibiotics don’t work
Most colds, flu, COVID-19, and sore throats come from viruses that antibiotics can’t treat or cure. Your immune system fights viral infections on its own, typically clearing them within 7 to 10 days. Taking antibiotics for viral infections wastes time, exposes you to unnecessary side effects, and creates resistant bacteria that threaten your health later. Rest, fluids, and over-the-counter medications manage your symptoms while your body battles the virus. You need antiviral medications, not antibiotics, for specific viral infections like influenza or herpes when treatment helps reduce severity or duration.
Mild bacterial infections your body can fight alone
Some bacterial infections clear up without antibiotics because your immune system effectively controls and eliminates the invading bacteria. Mild sinus infections often improve within 10 days without medication, though you might need antibiotics if symptoms persist or worsen. Minor ear infections in children over two years old frequently resolve on their own with pain management and monitoring. Small skin cuts with minimal redness and swelling heal with proper cleaning and bandaging rather than antibiotic treatment. Your doctor considers your overall health, age, and infection severity before deciding whether antibiotics provide more benefit than risk in these borderline cases.
Common infections antibiotics can treat
Doctors prescribe antibiotics for infections that bacteria cause and that pose serious health risks without treatment. Understanding which conditions require antibiotics helps you know when to seek medical care and what to expect from your doctor. Different bacteria cause different infections throughout your body, from your skin to your internal organs, and each requires specific antibiotic treatment. Your healthcare provider identifies the infection type through symptoms, physical examination, and sometimes lab tests before determining the right antibiotic for your situation.
Respiratory and throat infections
Strep throat requires antibiotic treatment because this bacterial infection spreads easily to others and can damage your heart or kidneys without proper care. Your doctor confirms strep through a rapid throat swab before prescribing antibiotics that make you non-contagious within 24 hours. Bacterial pneumonia needs antibiotics when bacteria infect your lungs, causing fever, chest pain, and difficulty breathing that won’t improve without medication. Whooping cough, also called pertussis, requires antibiotics to reduce severe coughing fits and prevent transmission to vulnerable people like infants.
Bacterial respiratory infections often need antibiotics to prevent serious complications and stop spreading to others.
Urinary tract and kidney infections
Urinary tract infections send millions of people to their doctors each year seeking relief from painful, frequent urination and lower abdominal discomfort. Bacteria entering your urinary system multiply rapidly and require antibiotics for infections that your body can’t eliminate through increased fluid intake alone. Kidney infections develop when urinary tract bacteria travel upward to your kidneys, causing fever, back pain, and nausea that demands immediate antibiotic treatment to prevent permanent kidney damage or life-threatening bloodstream infection.
Skin and soft tissue infections
Cellulitis requires prompt antibiotic treatment when bacteria enter through breaks in your skin and cause spreading redness, warmth, and swelling that penetrates deeper tissue layers. Impetigo, a highly contagious skin infection common in children, needs antibiotics to clear crusty sores and prevent spread to classmates or family members. Infected wounds from animal or human bites carry high contamination risk and require antibiotics to prevent serious complications like tetanus or blood infections. Staph infections, including MRSA, demand specific antibiotics that target these stubborn bacteria resistant to common medications.
Main types of antibiotics you may hear about
Doctors prescribe different antibiotic classes depending on which bacteria cause your infection and your individual health factors like allergies or other medications you take. Understanding these categories helps you recognize the names on your prescription bottle and know why your doctor chose a specific treatment for your condition. Each antibiotic class attacks bacteria in unique ways, from destroying their cell walls to disrupting their ability to make proteins they need to survive. Your pharmacist can explain more about your specific medication, but knowing the basics empowers you to ask better questions about your treatment.
Penicillins and beta-lactams
Penicillins rank as the most commonly prescribed antibiotics for infections and treat conditions ranging from strep throat to skin infections and urinary tract infections. Your doctor might prescribe amoxicillin for an ear infection or amoxicillin-clavulanate (Augmentin) for a sinus infection that needs broader bacterial coverage. These medications work by destroying bacterial cell walls, causing bacteria to break apart and die. Cephalosporins belong to the same beta-lactam family and serve as alternatives when you have mild penicillin allergies or need treatment for bacteria resistant to standard penicillins. Examples include cephalexin (Keflex) for skin infections and ceftriaxone for serious infections requiring injection.
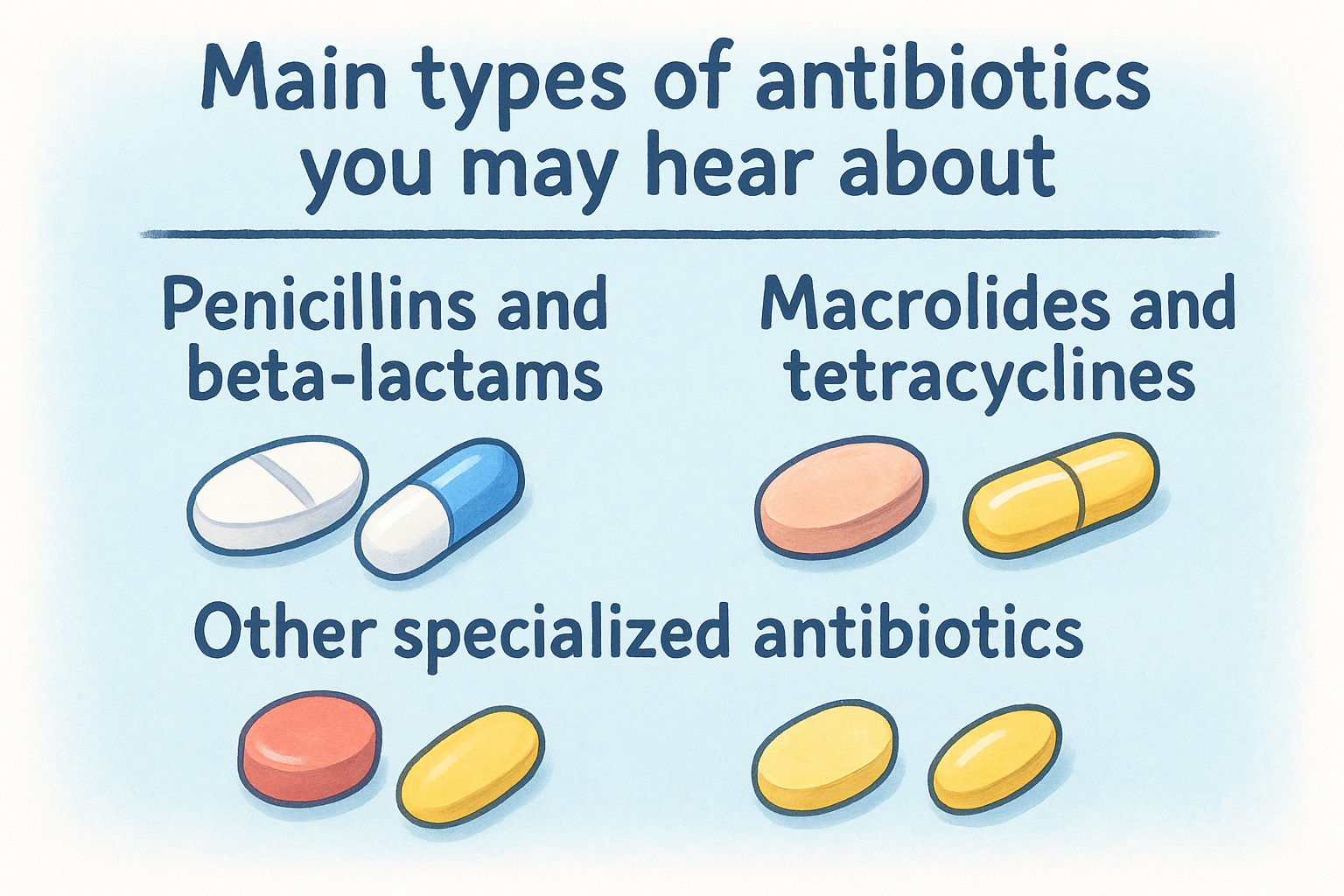
Macrolides and tetracyclines
Macrolides offer effective alternatives when you can’t take penicillins due to allergies or when bacteria don’t respond to first-line treatments. Azithromycin (Z-Pack) treats respiratory infections, whooping cough, and certain sexually transmitted infections through a convenient short-term course. Tetracyclines like doxycycline handle acne, Lyme disease, and some respiratory infections by preventing bacteria from making proteins they need to multiply.
Your doctor selects antibiotic classes based on which bacteria cause your infection and your personal health history.
Doctors avoid prescribing tetracyclines to pregnant women and young children because these medications can permanently discolor developing teeth and affect bone growth.
Other specialized antibiotics
Fluoroquinolones such as ciprofloxacin treat serious urinary tract infections and certain respiratory infections, but doctors now reserve them for specific situations because they carry risks of tendon damage and other serious side effects. Your provider prescribes these powerful medications only when safer alternatives won’t work effectively against your infection. Sulfonamides and aminoglycosides target specific bacterial infections that other antibiotics can’t eliminate, often requiring hospital administration for severe infections like sepsis or complicated kidney infections. Your healthcare team monitors you closely when you need these specialized treatments to ensure they work properly without causing dangerous side effects.
Side effects, risks and staying safe
Most people tolerate antibiotics well, but these powerful medications can cause side effects ranging from minor inconveniences to serious reactions requiring immediate medical attention. Understanding what to expect helps you distinguish between normal temporary discomfort and warning signs that demand professional care. Your risk of side effects increases when you take antibiotics incorrectly, combine them with certain other medications, or have underlying health conditions that affect how your body processes these drugs. Learning about common reactions and safety precautions protects you while ensuring antibiotics work effectively to clear your infection.
Common side effects you might experience
Digestive problems rank as the most frequent side effects from taking antibiotics, affecting your stomach and intestines as these medications kill both harmful and beneficial bacteria in your gut. Nausea, stomach pain, and loss of appetite typically resolve once you finish your prescription or improve when you take antibiotics with food. Diarrhea affects many people on antibiotics because these medications disrupt the natural balance of bacteria that help digest food in your intestines. Mild diarrhea usually improves within a few days, but severe or bloody diarrhea signals a potentially dangerous infection called C. diff that needs immediate medical evaluation.

Yeast infections develop in some women taking antibiotics because these medications eliminate protective bacteria that normally prevent fungal overgrowth in the vagina or mouth. Symptoms include itching, discharge, and discomfort that your doctor can treat with antifungal medication. Some antibiotics cause dizziness, headaches, or skin sensitivity to sunlight that requires extra sun protection while you complete your treatment. These mild side effects don’t typically require stopping your medication unless they become severe or interfere with your daily activities.
Minor side effects often improve as your body adjusts to the medication, but severe symptoms require medical attention.
Serious reactions that need immediate attention
Allergic reactions to antibiotics for infections create potentially life-threatening emergencies that demand immediate treatment. Severe reactions called anaphylaxis cause difficulty breathing, throat swelling, rapid heartbeat, and widespread rash developing within minutes to hours after taking your dose. Call 911 immediately if you experience these symptoms rather than waiting to contact your doctor or driving yourself to the emergency room. Milder allergic reactions produce itchy hives or skin rashes that still warrant a call to your healthcare provider to determine whether you should stop the antibiotic and switch to a different medication.
Severe diarrhea with blood or mucus, high fever, and intense abdominal cramping signal C. diff infection, a dangerous complication requiring different antibiotic treatment. Contact your doctor right away if diarrhea persists beyond a few days or worsens instead of improving. Some antibiotics damage tendons, particularly in people over 60, causing sudden pain or swelling in your joints that requires stopping the medication immediately to prevent rupture.
Drug interactions and safety precautions
Antibiotics interact with many common medications, reducing their effectiveness or creating dangerous side effects when taken together. Blood thinners, diabetes medications, and some heart drugs require dose adjustments or extra monitoring when combined with certain antibiotics. Tell your doctor and pharmacist about every medication, supplement, and vitamin you take before starting antibiotics to avoid potentially harmful interactions. Most antibiotics work safely with birth control pills, but some reduce contraceptive effectiveness and require backup protection during treatment.
Alcohol consumption with certain antibiotics causes severe nausea, vomiting, rapid heartbeat, and dangerous blood pressure changes that can land you in the emergency room. Your pharmacist provides specific guidance about whether you should avoid alcohol with your particular prescription. Store antibiotics properly at room temperature away from heat and moisture, and never share your prescription with family members who seem sick, even if their symptoms match yours.
What to remember
Antibiotics for infections save lives when used properly for bacterial conditions like strep throat, urinary tract infections, pneumonia, and serious skin infections that your immune system can’t fight alone. They won’t help viral infections such as colds, flu, or most sore throats, and taking them unnecessarily creates resistant bacteria that threaten everyone’s health in the future. Always complete your full prescription even after symptoms disappear, follow the timing and dosage instructions exactly as written, and never share your medication with family members or save leftover pills for future illnesses.
Your pharmacist serves as an essential partner throughout your antibiotic treatment, answering questions about potential side effects, dangerous drug interactions, and proper storage requirements that keep medications effective. Taking antibiotics correctly protects both your personal recovery and public health by preventing resistant bacteria from developing. Our team at Value Drugstore provides personalized consultations, prescription management, and expert guidance to ensure you use antibiotics safely and effectively for the best possible health outcomes.



