Managing a chronic illness often means taking medications every day for months or years. You might feel overwhelmed by all the options or worried about side effects that could build up over time. Maybe you have questions about whether your current medications are still right for you, or if there are safer alternatives you should know about. These concerns are valid and worth exploring.
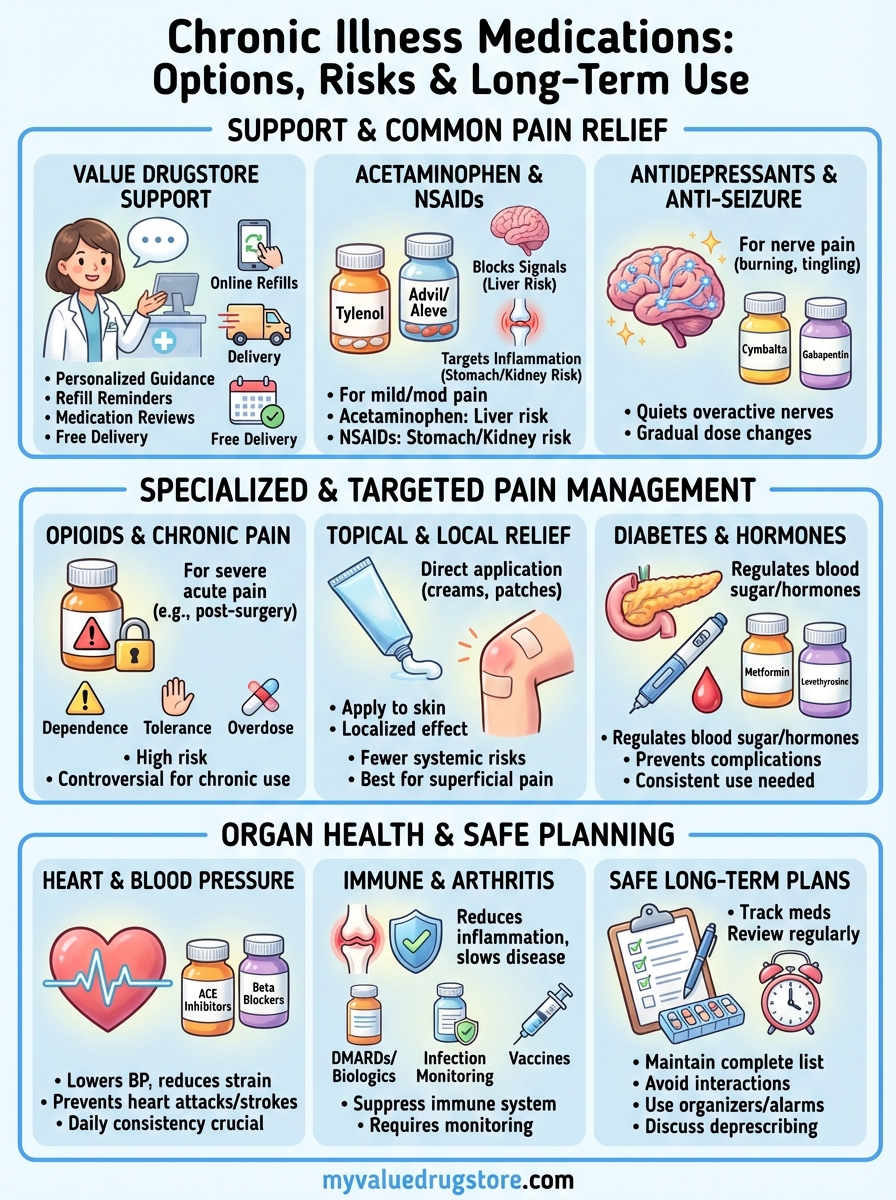
This guide breaks down the most common medications used for chronic conditions like pain, diabetes, heart disease, and arthritis. You will learn how each type of medication works, what benefits it offers, and what risks you need to watch for during long term use. We cover everything from over the counter pain relievers to prescription opioids, heart medications, and immune suppressing drugs. You will also find practical advice on building a safe medication routine, avoiding dangerous interactions, and working with your pharmacist to get the most from your treatment plan. Whether you are starting your first chronic medication or reviewing a list you have been taking for years, this information will help you make informed decisions about your care.
1. Value Drugstore medication support
Managing chronic illness medications becomes easier when you have a local pharmacy team that knows your health history and treatment goals. Value Drugstore offers personalized support that goes beyond simply filling prescriptions, helping you navigate the complexities of long term medication use with expert guidance and convenient services tailored to your needs.
How Value Drugstore supports chronic medications
Your pharmacists at Value Drugstore track your complete medication profile and watch for interactions or duplicate therapies that could cause harm. They answer questions about dosing schedules, side effects, and how your medications work together. This ongoing relationship means someone familiar with your case is always available to help you stay on track.
Services that simplify refills and delivery
You can refill prescriptions online through a secure platform and have medications delivered to your door at no extra cost. Automatic refill reminders prevent gaps in your treatment, which is especially important for chronic conditions that require consistent medication levels.
When to schedule a medication review
Schedule a review when you start a new chronic medication, notice unusual side effects, or add any over the counter supplements to your routine. Annual reviews help ensure your treatment plan still matches your current health status and goals.
Regular medication reviews catch problems before they become serious and help you get the most benefit from each drug.
Questions to ask your local pharmacist
Ask about the best time to take each medication, which foods or drinks to avoid, and what side effects need immediate attention. Request information about cost saving options and whether generic alternatives would work as well for your condition.
2. Acetaminophen and anti inflammatory medicines
Acetaminophen and nonsteroidal anti inflammatory drugs (NSAIDs) are often the first line of defense against mild to moderate chronic pain from conditions like arthritis, back injuries, and muscle inflammation. These medications work differently in your body, and understanding each type helps you choose the safest option for long term management of your symptoms.
How these pain relievers work
Acetaminophen blocks pain signals in your central nervous system without reducing inflammation at the injury site. NSAIDs like ibuprofen and naproxen target COX enzymes that create prostaglandins, the chemicals responsible for both pain and inflammation in damaged tissues. This dual action makes NSAIDs more effective when your pain comes from swollen joints or inflamed muscles.
Common drugs and when to use each
Acetaminophen (Tylenol) works best for headaches, fever, and pain without significant swelling. Ibuprofen (Advil, Motrin) and naproxen (Aleve) relieve arthritis pain, menstrual cramps, and injuries where inflammation plays a key role. Celecoxib (Celebrex), a COX 2 inhibitor, offers similar relief with less stomach irritation for people who need daily NSAID therapy.
Benefits, risks and side effects
You can purchase these chronic illness medications without a prescription and find quick relief for many pain types. NSAIDs may cause stomach bleeding, ulcers, or kidney problems when taken long term or at high doses. Acetaminophen in excessive amounts damages your liver, especially when combined with alcohol.
Taking more than the recommended dose rarely brings better pain relief and dramatically increases your risk of serious organ damage.
When to avoid or limit these medicines
Avoid NSAIDs if you have kidney disease, stomach ulcers, or heart failure. Limit acetaminophen to 3,000 milligrams daily and check every medication label for hidden acetaminophen in combination products. Your age, other medications, and existing health conditions all affect whether these drugs remain safe for your daily chronic pain management.
3. Antidepressants and anti seizure medicines
Antidepressants and anti seizure medications treat chronic pain by quieting overactive nerve signals that keep firing long after an injury heals. These chronic illness medications work particularly well for burning, shooting, or tingling pain from nerve damage caused by diabetes, shingles, spinal cord injuries, or fibromyalgia. Your provider may prescribe them even if you do not have depression or seizures.
How they help with chronic and nerve pain
Nerve pain occurs when damaged nerves send constant distress signals to your brain. Antidepressants increase certain brain chemicals that turn down pain volume throughout your nervous system. Anti seizure medications stabilize nerve cell membranes to prevent the electrical misfires that create chronic pain sensations.
Examples your provider may suggest
Tricyclic antidepressants like amitriptyline and nortriptyline work at low doses to relieve nerve pain and improve sleep quality. SNRIs (serotonin norepinephrine reuptake inhibitors) such as duloxetine (Cymbalta) and venlafaxine (Effexor) treat both pain and mood symptoms. Gabapentin (Neurontin) and pregabalin (Lyrica) address the burning pain of shingles and diabetic neuropathy.
Benefits, side effects and monitoring
These medications offer pain relief without the addiction risks of opioids and help many people regain function. Side effects include dizziness, drowsiness, and nausea, though bedtime dosing reduces daytime tiredness. Regular follow ups catch rare mood changes that require immediate medical attention.
These medications need several weeks of consistent daily use before you notice their full pain relieving effects.
What to expect when starting or stopping
Your provider starts you on a low dose and slowly increases it over weeks to find the smallest effective amount. Stopping suddenly causes withdrawal symptoms, so you work with your care team to gradually taper the dose when it is time to discontinue treatment.
4. Opioid medications and chronic pain
Opioid medications provide powerful relief for severe acute pain but create complex challenges when used for chronic conditions. These drugs include hydrocodone, oxycodone, morphine, and fentanyl, which attach to receptors in your brain to block pain signals and alter your emotional response to discomfort. Long term opioid use for chronic pain remains controversial because research shows declining effectiveness over time while risks of serious complications continue to increase.
How opioids relieve pain and their limits
Opioids mimic your body’s natural endorphins to reduce pain intensity and create feelings of calm or euphoria. Your nervous system adapts within weeks, requiring higher doses to achieve the same pain relief through a process called tolerance. This ceiling effect means you face greater risks without proportional pain control, especially when managing conditions that last months or years.
When opioids may be considered
Your provider may prescribe opioids for cancer related pain or severe acute injuries like broken bones or post surgical recovery. These chronic illness medications serve as a last resort when other treatments have failed completely for noncancer chronic pain. Careful screening for addiction risk factors guides decisions about whether opioid therapy makes sense for your specific situation.
Risks of dependence and overdose
Physical dependence develops quickly, causing withdrawal symptoms if you stop suddenly or miss doses. Addiction involves compulsive use despite harmful consequences and affects a percentage of chronic opioid users. Overdose deaths from opioids continue rising nationwide, with respiratory depression representing the most dangerous acute risk.
Even a five day prescription increases your odds of still taking opioids one year later, highlighting how quickly dependence can develop.
Safer use, tapering and alternatives
Take opioids exactly as prescribed and store them securely away from others in your household. Gradual tapering under medical supervision prevents severe withdrawal when discontinuing treatment. Alternative approaches like physical therapy, nerve blocks, and non opioid chronic illness medications often provide better long term outcomes without addiction risks.
5. Topical and local pain relief
Topical pain relievers apply medication directly to your skin over the painful area, delivering relief without systemic side effects that oral chronic illness medications can cause. These treatments include creams, gels, patches, and sprays that work locally to reduce inflammation and block pain signals at the source. You avoid many risks of liver, kidney, or stomach damage when medication stays confined to the application site.
Types of topical and local treatments
Lidocaine patches numb nerve endings in your skin for localized pain from shingles or nerve injuries. Capsaicin creams from hot peppers deplete pain transmitters after several applications. NSAID gels like diclofenac penetrate inflamed joints without exposing your entire digestive system to the drug.
When they work best for chronic pain
You gain the most benefit when pain affects superficial areas close to your skin surface, such as arthritic knees, sore muscles, or specific nerve pain zones. Deep joint pain or widespread conditions respond less reliably because topical medications cannot reach tissues far below the skin.
Safety tips for creams patches and gels
Apply products only to intact skin without cuts or rashes. Wash your hands thoroughly after each use to prevent accidental contact with eyes or mucous membranes. Heating pads should never combine with topical medications because heat increases absorption and risk of burns.
Topical treatments let you target specific pain areas while minimizing the medication burden on your liver and kidneys.
Combining topical and oral medicines
You can safely layer topical relief with oral medications when pain requires multiple approaches. Check ingredient lists carefully to avoid doubling up on the same active drug in both topical and oral forms.
6. Medications for diabetes and hormones
Diabetes and hormonal disorders require daily medications that regulate critical body functions like blood sugar levels, metabolism, and growth. These chronic illness medications work continuously to prevent complications that develop when hormones fall too high or too low for extended periods. Your treatment plan often combines multiple drugs to achieve stable control while minimizing side effects that could affect your quality of life.
Main types of diabetes medications
Metformin lowers blood sugar by reducing glucose production in your liver and improving insulin sensitivity in your muscles. Insulin injections replace or supplement the hormone your pancreas cannot produce in adequate amounts. Newer drugs like GLP 1 agonists and SGLT2 inhibitors help your body release insulin, slow digestion, or remove excess glucose through urine.
Medicines for thyroid and hormone balance
Levothyroxine replaces thyroid hormone when your gland produces too little, affecting metabolism and energy levels. Hormone replacement therapy restores estrogen or testosterone to healthy ranges during menopause or age related decline. Consistency in taking these medications at the same time daily maintains stable hormone levels your body needs to function properly.
Long term risks and benefits to know
Diabetes medications prevent blindness, kidney failure, and nerve damage by keeping blood sugar in healthy ranges. Some drugs cause weight gain, digestive upset, or low blood sugar episodes that require immediate treatment. Regular monitoring through blood tests tracks organ function and adjusts dosing before problems develop.
Consistent medication use combined with lifestyle changes gives you the best protection against diabetes complications over your lifetime.
Working with your care team on targets
Your provider sets personalized targets for blood sugar, A1C levels, and other markers based on your age, overall health, and complication risks. Schedule appointments every three to six months to review your numbers and adjust medications when needed. Ask about medication timing relative to meals and whether generic options would reduce your costs without affecting results.
7. Medications for heart and blood pressure
Heart disease and high blood pressure rank among the leading causes of death worldwide, making cardiovascular medications some of the most commonly prescribed chronic illness medications. These drugs work through various mechanisms to reduce strain on your heart, lower blood pressure, and prevent life threatening complications like heart attacks and strokes. Your treatment plan may include one or several medications taken daily to keep your cardiovascular system functioning optimally for years to come.
Key blood pressure and heart medications
ACE inhibitors and ARBs (angiotensin receptor blockers) relax blood vessels by blocking hormones that tighten them, making it easier for your heart to pump blood throughout your body. Beta blockers slow your heart rate and reduce the force of contractions to decrease blood pressure and oxygen demand. Calcium channel blockers prevent calcium from entering heart and blood vessel cells, causing vessels to widen and blood pressure to drop. Diuretics remove excess fluid through your kidneys to reduce blood volume and pressure on artery walls.

How these drugs protect you over time
Consistent medication use keeps your blood pressure below 130/80 mmHg, the threshold where damage to arteries, kidneys, and eyes accelerates significantly. Long term control reduces your stroke risk by 40 percent and heart attack risk by 25 percent compared to untreated hypertension. These protective benefits accumulate gradually, requiring months or years of adherence before you see the full reduction in cardiovascular events.
Missing even a few doses can cause dangerous blood pressure spikes that strain your heart and increase your immediate risk of stroke or heart attack.
Side effects that need prompt attention
Watch for dizziness when standing up, persistent dry cough, or swelling in your ankles that worsens over days. Irregular heartbeat, severe fatigue, or fainting episodes require immediate medical evaluation. Report any new symptoms promptly so your provider can adjust your medication before complications develop.
Tips to never miss a heart medication dose
Link your medication schedule to daily routines like brushing your teeth or eating breakfast to build automatic habits. Use pill organizers with compartments for each day of the week and set phone alarms as backup reminders. Request auto refills through Value Drugstore so your supply never runs out between pharmacy visits.
8. Immune and arthritis medicines
Arthritis and autoimmune conditions like rheumatoid arthritis, lupus, and psoriatic arthritis require chronic illness medications that reduce inflammation and slow disease progression. These drugs work by dampening your immune system’s attack on healthy tissues, which relieves joint pain and prevents permanent damage to your bones and organs. Your treatment plan often starts with milder medications and progresses to stronger immune suppressing drugs when your condition demands more aggressive control.
Anti inflammatory drugs for arthritis
NSAIDs like ibuprofen, naproxen, and celecoxib provide the first line of defense against arthritis pain and swelling in your joints. These medications reduce inflammation quickly but do not stop your disease from progressing over time. Your provider may prescribe higher prescription doses than over the counter versions when inflammation proves difficult to control with standard amounts.
Disease modifying and biologic medicines
Disease modifying antirheumatic drugs (DMARDs) such as methotrexate and hydroxychloroquine slow arthritis progression by suppressing parts of your immune system that attack joints. Biologic medications target specific immune proteins like TNF alpha or interleukins that drive inflammation throughout your body. These powerful drugs often bring dramatic relief when other treatments fail, though they take weeks or months to reach full effectiveness.
Infection and lab monitoring needs
Your weakened immune system makes you more vulnerable to infections while taking these medications. Schedule blood tests every three to six months to check liver function, kidney health, and blood cell counts that can drop dangerously low. Report fever, persistent cough, or unusual fatigue immediately because infections can escalate rapidly when your immune defenses are suppressed.
Regular lab monitoring catches problems before they become serious, allowing your provider to adjust your medication or add protective treatments.
Vaccines and precautions with immune drugs
Complete recommended vaccines before starting biologic therapy because live vaccines become unsafe once you begin immune suppression. Schedule your annual flu shot and stay current with pneumonia vaccines to reduce your infection risk. Discuss timing with your provider since some vaccines work best when given between medication doses rather than during active treatment.
9. Safe long term medication plans
Creating a safe medication plan for chronic conditions requires more than simply taking pills on schedule every day. You need a clear system that tracks every drug you take, catches potential problems before they harm you, and adapts as your health needs change over months and years. A well organized approach to your chronic illness medications reduces your risk of dangerous interactions while helping you stay consistent with treatments that protect your health.
Building a complete medication list
Write down every medication you take, including prescriptions, over the counter drugs, vitamins, supplements, and herbal remedies. Record the name, dose, and schedule for each item along with the reason you take it. Keep copies in your wallet, on your phone, and share an updated version with every provider you see.

Avoiding dangerous interactions
Your complete medication list helps pharmacists spot problems when drugs interfere with each other or worsen existing conditions. Certain combinations increase bleeding risk, cause dangerous heart rhythms, or trigger severe allergic reactions. Review your list at every appointment and before adding any new medication or supplement to your routine.
A single pharmacy that fills all your prescriptions provides the best safety net against dangerous drug interactions.
Tools and habits that support adherence
Pill organizers with daily compartments prevent confusion about which doses you have already taken. Phone alarms serve as reliable reminders when your schedule varies from day to day. Linking medication times to established routines like meals makes adherence automatic rather than requiring constant mental effort.
When to ask about deprescribing
Request a medication review when you take five or more chronic illness medications, experience frequent falls or confusion, or notice side effects that reduce your quality of life. Some medications become unnecessary as your health improves or may cause more harm than benefit as you age. Your provider can safely eliminate or reduce drugs that no longer serve your current health goals.
Next steps for your medications
Your chronic illness medications work best when you understand how they function, what risks they carry, and how to take them safely over months or years. This knowledge helps you have better conversations with your healthcare team and spot problems before they become serious. Regular medication reviews catch interactions and outdated treatments that might harm you.
Building a strong relationship with your local pharmacy creates an extra safety net for your health. Value Drugstore offers personalized support that goes beyond filling prescriptions, with pharmacists who know your complete medication history and can answer questions about new symptoms or drug interactions. You gain convenient services like free delivery, online refills, and medication reviews that make long term treatment easier to manage.
Start by organizing your complete medication list and scheduling your next pharmacy consultation to review your current chronic illness medications together.



