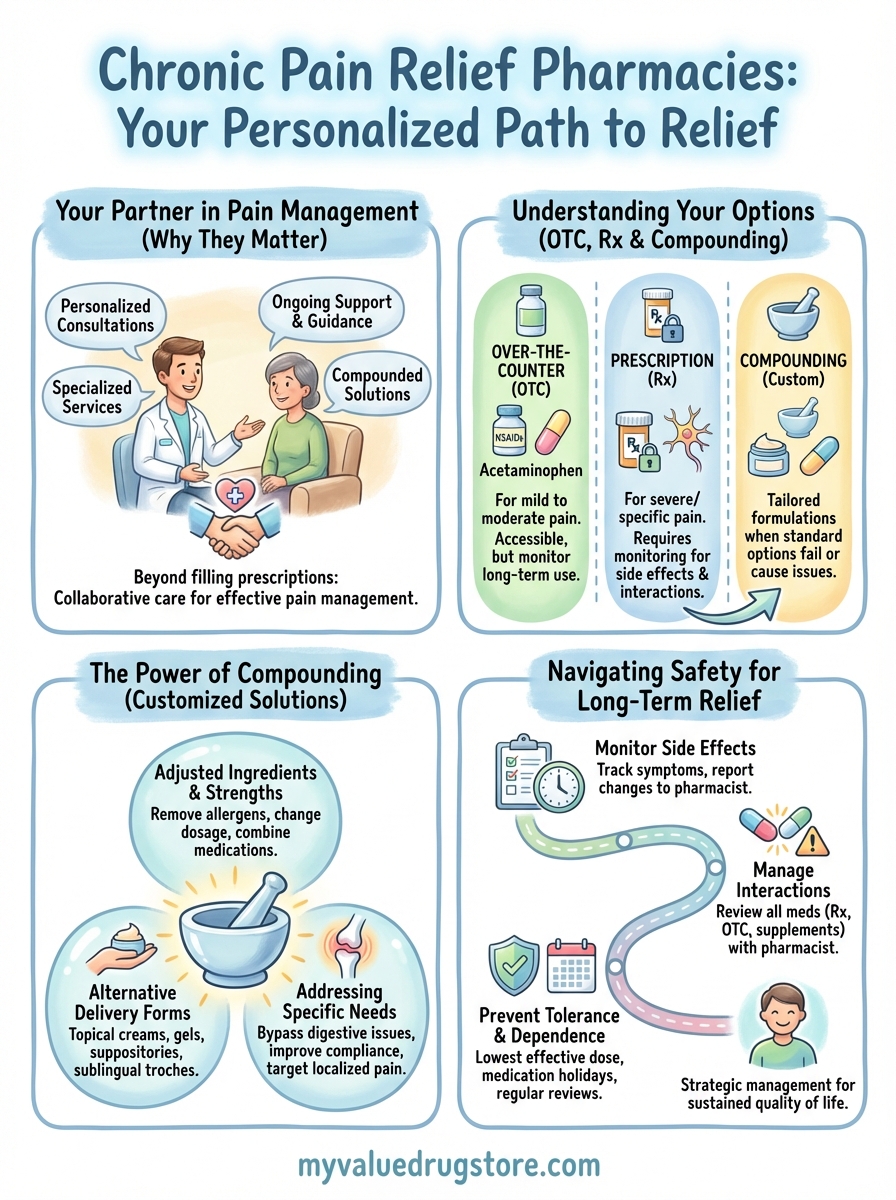
A chronic pain relief pharmacy is a pharmacy that specializes in helping you manage ongoing pain through prescription medications, over the counter products, and customized compounded treatments. Unlike a standard drugstore that only fills prescriptions, these pharmacies offer personalized consultations, alternative dosage forms, and specialized services that address your specific pain management needs. Many independent pharmacies provide compounding services that can create customized pain medications when standard options cause side effects or don’t work for you.
This guide walks you through how pharmacies can help with chronic pain relief. You’ll learn the difference between over the counter and prescription options, when compounding makes sense, how to work with your pharmacist for better results, and safety considerations for long term pain medication use. Whether you’re dealing with arthritis, nerve pain, fibromyalgia, or other chronic conditions, understanding your pharmacy options helps you make informed decisions about pain management that fits your life.
Why chronic pain relief pharmacies matter
Chronic pain affects more than 100 million Americans, yet many people struggle to find relief because standard treatments don’t address their individual needs. A chronic pain relief pharmacy offers specialized services that go beyond simply filling prescriptions. These pharmacies provide personalized consultations, compounded medications, and ongoing support that helps you manage pain more effectively. Your pharmacist becomes a partner in your care, working alongside your doctor to find solutions that actually work for your specific condition and lifestyle.

Personalized pain management solutions
Standard pain medications come in fixed doses and forms that don’t work for everyone. Compounding pharmacies create customized formulations that match your exact needs, whether you need a different strength, a topical cream instead of a pill, or a combination of medications in one dose. This personalization reduces side effects and improves results because the medication fits your body instead of forcing you to adapt to a one-size-fits-all product.
Your pain is unique, and your treatment should reflect that reality. Specialized pharmacies can adjust ingredients to remove allergens, add flavoring for easier use, or create alternative delivery methods like gels or suppositories. These options matter when oral medications cause stomach problems or when you need pain relief applied directly to the affected area.
Access to expert guidance
Pharmacists at pain management focused pharmacies understand how different medications interact with your body and with each other. They spend time reviewing your complete medication list, identifying potential problems, and suggesting adjustments that your doctor might not catch during a brief office visit. This expertise prevents dangerous drug interactions and helps you avoid medications that could worsen your condition.
The right pharmacy partnership transforms pain management from a guessing game into a strategic plan.
Your pharmacist tracks your progress and notices patterns that might indicate a need to change medications or dosages. They provide practical advice about timing doses, managing side effects, and knowing when to call your doctor. This ongoing support fills the gap between doctor appointments and gives you someone accessible to answer questions as they arise. Finding a pharmacy that prioritizes patient education and personalized care means you get better outcomes and fewer frustrating setbacks in managing chronic pain.
How to use a pharmacy for chronic pain care
Using a chronic pain relief pharmacy effectively starts with choosing the right pharmacy and building a relationship with your pharmacist. You need more than a place that fills prescriptions quickly. Look for pharmacies that offer consultation services, compounding capabilities, and pharmacists who take time to understand your specific pain condition. Independent pharmacies often provide this level of personalized care better than large chains where staff turnover runs high and pharmacists juggle hundreds of prescriptions daily.
Starting the conversation with your pharmacist
Schedule a consultation appointment instead of trying to discuss your pain management during busy pickup hours. Bring your complete medication list, including supplements and over the counter products, because your pharmacist needs the full picture to identify potential interactions or duplications. Explain your pain patterns, what triggers flare-ups, and which treatments you’ve already tried. This information helps your pharmacist recommend appropriate options and flag concerns your doctor should address.

Ask specific questions about timing, food interactions, and what to expect from new medications. Your pharmacist can explain why certain medications work better at night or need to be taken with food, details that improve results and reduce side effects. They also know which generic versions work as well as brand names and which ones patients report problems with, information that saves you money and frustration.
Building an ongoing relationship
Track your results and report back regularly to your pharmacist about what’s working and what isn’t. This feedback helps them fine tune recommendations and catch problems early. Your pharmacist notices patterns across their patient population and can warn you about emerging issues with specific medications or suggest alternatives when shortages affect your usual prescription. They become your advocate, contacting your doctor when medications need adjustment or prior authorizations hit roadblocks.
Consistent communication with your pharmacist turns pain management from trial and error into a coordinated strategy.
Request medication reviews every six months or when your pain treatment changes. These reviews catch outdated prescriptions, identify medications you no longer need, and ensure new additions don’t conflict with existing treatments. Your pharmacist can also connect you with support resources, patient assistance programs for expensive medications, and local specialists who focus on chronic pain management. This partnership approach gives you someone accessible who understands your complete pain management picture and works to optimize every aspect of your treatment.
Comparing OTC and prescription pain options
Understanding the difference between over the counter and prescription pain medications helps you make informed choices at your chronic pain relief pharmacy. OTC medications work well for mild to moderate pain and offer convenience since you can purchase them without a doctor’s visit. Prescription medications target more severe or specific types of chronic pain that don’t respond to standard treatments. Your pharmacist can explain which option fits your pain level, how long you’ve been dealing with discomfort, and whether your condition requires stronger intervention or specialized formulations.
Understanding over the counter pain relievers
OTC pain medications fall into two main categories: NSAIDs like ibuprofen and naproxen, and acetaminophen products like Tylenol. NSAIDs reduce both pain and inflammation, making them effective for arthritis, muscle strains, and pain with swelling. They work by blocking enzymes that cause inflammation in your body. Acetaminophen relieves pain without addressing inflammation, which makes it better for headaches or pain without swelling but less effective for inflammatory conditions.
You can use OTC medications for acute flare-ups or mild chronic pain without needing a prescription. These options cost less and allow you to start treatment immediately. However, long term use of NSAIDs can cause stomach problems, ulcers, or kidney issues, especially at higher doses. Acetaminophen taken in large amounts or combined with alcohol damages your liver over time. Your pharmacist tracks these risks and warns you when OTC use becomes problematic or when you need stronger alternatives.
When prescription medications become necessary
Prescription pain medications become essential when OTC options fail to control your pain or when your condition requires targeted treatment. Opioids like hydrocodone or oxycodone provide powerful relief for severe acute pain following surgery or injury, but doctors rarely prescribe them long term due to addiction risks and tolerance issues. Nerve pain medications like gabapentin or duloxetine work specifically on damaged nerves and treat conditions like diabetic neuropathy or fibromyalgia that don’t respond to standard painkillers.
Prescription options also include muscle relaxants, topical formulations, and combination medications that address multiple pain mechanisms simultaneously. Your doctor prescribes these when they understand your specific diagnosis and pain patterns. Prescription medications require monitoring because they carry higher risks of side effects, interactions with other drugs, and dependency concerns. Your pharmacist reviews these prescriptions carefully and contacts your doctor if dosages seem inappropriate or if dangerous combinations appear in your medication profile.
Prescription medications offer stronger relief but demand closer supervision than over the counter options.
Making the right choice for your situation
Start with OTC options for new or mild pain episodes before moving to prescription medications. This approach lets you gauge whether simple treatments solve the problem and avoids unnecessary exposure to stronger drugs with more side effects. Track your pain levels, how long relief lasts, and any side effects you experience. This information helps your pharmacist and doctor determine if you need to escalate treatment or try different approaches.
Prescription medications make sense when OTC products stop working, when side effects from high dose OTC use become concerning, or when your pain significantly limits daily activities despite trying standard treatments. Your pharmacist helps you understand these decision points and ensures smooth transitions between treatment levels.
What to know about compounding for pain
Compounding creates customized pain medications tailored to your specific needs when standard manufactured products don’t work or cause unwanted side effects. A compounding pharmacist prepares medications from scratch using individual pharmaceutical ingredients, adjusting strengths, changing delivery forms, or combining multiple drugs into one dose. This process gives you access to treatment options unavailable through commercial manufacturers, addressing problems like allergies to inactive ingredients, difficulty swallowing pills, or the need for pain relief applied directly to affected areas rather than taken systemically.
When compounding makes sense for pain relief
You benefit from compounded pain medications when standard treatments cause intolerable side effects or fail to provide adequate relief. Patients who experience severe stomach upset from oral NSAIDs can get the same medication as a topical gel applied directly to painful joints, bypassing the digestive system entirely. Compounding solves problems with discontinued medications that worked well for you, allergies to dyes or preservatives in commercial products, or when you need a strength between available manufactured doses.
Chronic conditions often require multiple pain medications taken at different times, which becomes difficult to manage and reduces compliance. Compounding pharmacies combine these medications into a single dose form, simplifying your routine and improving consistency. Patients with nerve pain might need both an anti-inflammatory and a nerve pain medication applied to the same area, which compounding delivers in one cream rather than juggling separate products.
Common compounded pain formulations
Topical pain creams and gels represent the most popular compounded formulations because they deliver medication directly to painful areas with minimal systemic absorption. Your pharmacist can combine ingredients like ketoprofen, gabapentin, lidocaine, and muscle relaxants into one topical preparation that addresses multiple pain mechanisms simultaneously. These formulations work well for localized arthritis pain, neuropathy, or muscle injuries where you want concentrated relief without affecting your entire body.

Compounded formulations give you treatment options that commercial manufacturers don’t provide because they address individual needs rather than mass market demands.
Alternative delivery forms include suppositories for patients who cannot swallow or have nausea, sublingual troches that dissolve under your tongue for faster absorption, or transdermal patches for steady medication release throughout the day. Flavored suspensions help patients who struggle with bitter tasting medications, while preservative-free formulations prevent allergic reactions in sensitive individuals. Your chronic pain relief pharmacy can create capsules with precise custom strengths when available doses don’t match your needs.
Getting compounded medications
You need a prescription from your doctor specifically written for compounding since these medications require individualized preparation. Your physician works with your compounding pharmacist to determine the right formulation, strength, and ingredients for your condition. Insurance coverage varies significantly, with some plans covering compounded medications and others requiring out-of-pocket payment, so verify coverage before filling your prescription to avoid unexpected costs.
Compounded medications take longer to prepare than standard prescriptions because pharmacists create each batch individually. Allow 24 to 48 hours for preparation rather than expecting same day pickup. Store compounded medications according to your pharmacist’s instructions since they lack the preservatives and stabilizers found in commercial products, which affects shelf life and storage requirements.
Safety tips for long term pain medicines
Long term pain medication use requires careful monitoring and strategic management to prevent serious health problems. Your body adapts to medications over time, which can reduce effectiveness, create dependency, or cause cumulative damage to organs like your liver and kidneys. Regular check-ins with your chronic pain relief pharmacy help catch problems early and adjust your treatment before complications develop. You need specific strategies to use pain medications safely for months or years while maintaining quality of life and protecting your overall health.
Monitoring for side effects and complications
Track new symptoms or changes in how you feel after starting pain medications or increasing dosages. Write down when side effects occur, how severe they are, and whether they improve or worsen over time. Common problems include stomach upset, dizziness, constipation, or drowsiness, but serious complications like bleeding, confusion, or difficulty breathing require immediate medical attention. Your pharmacist reviews these patterns and determines whether side effects are temporary adjustments or signs that you need different medications.
Schedule regular lab work to monitor organ function when taking medications that stress your liver or kidneys. NSAIDs taken daily for months can damage kidneys or raise blood pressure, while acetaminophen accumulates and harms your liver if you exceed safe daily limits. Blood tests catch these problems before they become irreversible, allowing your doctor to switch medications or adjust doses. Your pharmacy tracks refill dates and can alert you when monitoring appointments are overdue.
Regular monitoring turns long term medication use from a risk into a managed strategy.
Managing medication interactions
Review your complete medication list with your pharmacist every time you add or remove a drug, including prescriptions, over the counter products, and supplements. Pain medications interact with blood thinners, blood pressure drugs, antidepressants, and many other common treatments in ways that increase side effects or reduce effectiveness. Your pharmacist catches dangerous combinations before they cause problems, something that’s difficult when you see multiple doctors who don’t communicate about your full medication picture.
Avoid alcohol when taking acetaminophen or opioid pain medications because it multiplies liver damage risks and increases sedation to dangerous levels. Some pain medications interact with specific foods or require taking with meals to prevent stomach damage. Understanding these interactions helps you use medications safely and get consistent results.
Preventing tolerance and dependence
Your body adapts to pain medications taken daily, requiring higher doses for the same relief. This tolerance develops faster with opioids but also occurs with other pain medications over time. Work with your doctor to schedule medication holidays or rotate between different pain relievers to maintain effectiveness. These breaks prevent your body from becoming completely dependent on one medication and reduce the risk of addiction with controlled substances.
Use pain medications at the lowest effective dose for the shortest time needed to control symptoms. Take them on schedule for severe chronic pain rather than waiting until pain becomes unbearable, which prevents the cycle of under-medicating and over-medicating that leads to tolerance. Your pharmacist helps you balance adequate pain control with the goal of using the minimum medication necessary.
Next steps
Managing chronic pain requires a pharmacy partner who understands your specific needs and provides personalized solutions beyond simply filling prescriptions. Start by scheduling a consultation with a pharmacist who specializes in pain management to review your current medications, discuss alternative options, and explore whether compounding could improve your results. Bring your complete medication list and be prepared to explain what works, what doesn’t, and what side effects limit your daily activities.
Your chronic pain relief pharmacy becomes most valuable when you build an ongoing relationship through regular communication and medication reviews. Track your pain levels, side effects, and any changes in your condition so your pharmacist can adjust recommendations and work with your doctor to optimize treatment. Finding a pharmacy committed to personalized care and patient education transforms pain management from frustrating trial and error into a strategic partnership. Learn more about our commitment to personalized pharmacy services and how we support your pain management journey with accessible, quality care tailored to your individual needs.



