Understanding Drug Interactions: What You Need to Know

Understanding Drug Interactions: What You Need to Know to Use Medications Safely
Written by: Dr. Sarah Chen, Pharm.D., 12 years of experience in clinical pharmacy
Medically Reviewed by: Dr. Michael Lee, M.D.
Last Medical Review: October 26, 2023
Dr. Lee is a board-certified physician with extensive experience in medication management and patient safety. His expertise ensures the accuracy and clinical relevance of the information presented in this guide, adhering to the highest medical standards and current medical guidelines.

Drug interactions happen when one medication, supplement, or food changes how another works — either by altering its effect or its level in your body. Knowing how interactions happen helps you avoid harm and get the best results from treatment, ensuring overall medication safety. This guide, informed by clinical experience and medical guidelines, breaks down the main interaction types, explains the clinical mechanisms in plain language, and highlights who is most at risk (for example, older adults, people taking many medicines, or anyone using herbal supplements). You’ll find real-world examples of high-risk drug pairs, common food and supplement conflicts to watch for, and simple everyday steps to lower your chance of an adverse reaction. The article also covers when to call a pharmacist for expert pharmacy advice, how telehealth medication reviews work, and how community pharmacies can manage interactions without creating extra hassle. Finally, see how Value Drugstore’s pharmacy services support medication safety through medication reconciliation, compounding, refills, and telehealth consultations to help you follow these prevention tips more easily.
What Are the Different Types of Drug Interactions?
Drug interactions fall into three practical categories: drug-drug, drug-food/drink, and drug-condition interactions. They work in different ways — pharmacokinetic interactions change how the body absorbs, distributes, metabolizes, or clears a drug, while pharmacodynamic interactions change how drugs act at the same receptor or body pathway. Both can make a medicine less effective or increase the chance of harm. Knowing these categories helps you and your clinician predict problems and choose safer options or monitoring plans, a key aspect of medication safety. The short list below defines each type so you can spot them quickly.
- Drug-drug interactions: One medicine changes the level or effect of another through metabolism or additive effects.
- Drug-food/drink interactions: Foods or beverages alter medication levels or actions — for example, grapefruit or vitamin K–rich greens.
- Drug-condition interactions: An existing health problem (like kidney disease) changes how a drug behaves or raises its risk.
These quick definitions set the stage for the deeper explanations and examples that follow, providing a foundation for understanding potential drug interactions.
How Do Drug-Drug Interactions Affect Medication Safety?
Drug-drug interactions occur when one medicine alters another’s absorption, metabolism, excretion, or receptor activity. The result can be reduced benefit or increased side effects. A common pathway involves liver enzymes in the CYP family: one drug can speed up (induce) or slow down (inhibit) the metabolism of another, lowering its effect or raising its toxicity. Clinically important examples include combinations that increase bleeding risk or cause dangerous breathing suppression when sedatives and opioids are used together. People taking many medicines (polypharmacy), those with impaired kidney or liver function, or patients seeing multiple prescribers are at higher risk. Regular medication review and careful monitoring, guided by expert pharmacy advice, are key to preventing harm and ensuring medication safety. Next, we’ll look at drug-food interactions, which often complicate these scenarios further.
Pharmacokinetic Drug-Drug Interactions and Clinical Management
Drug–drug interactions are a frequent source of medication error—particularly among older adults on multiple therapies—reported in studies with prevalence estimates around 20–40%. Poly-therapy increases the complexity of treatment and the chance of clinically important interactions, which can either cause adverse reactions or reduce a drug’s benefit. Most interactions fall into pharmacokinetic or pharmacodynamic groups. This review searched Medline, PubMed, Embase, the Cochrane Library and reference lists through June 30, 2012, and focuses on mechanisms and clinical implications of pharmacokinetic DDIs.
Pharmacokinetic drug-drug interaction and their implication in clinical management, A Di Paolo, 2013
What Are Common Drug-Food and Drug-Beverage Interactions?
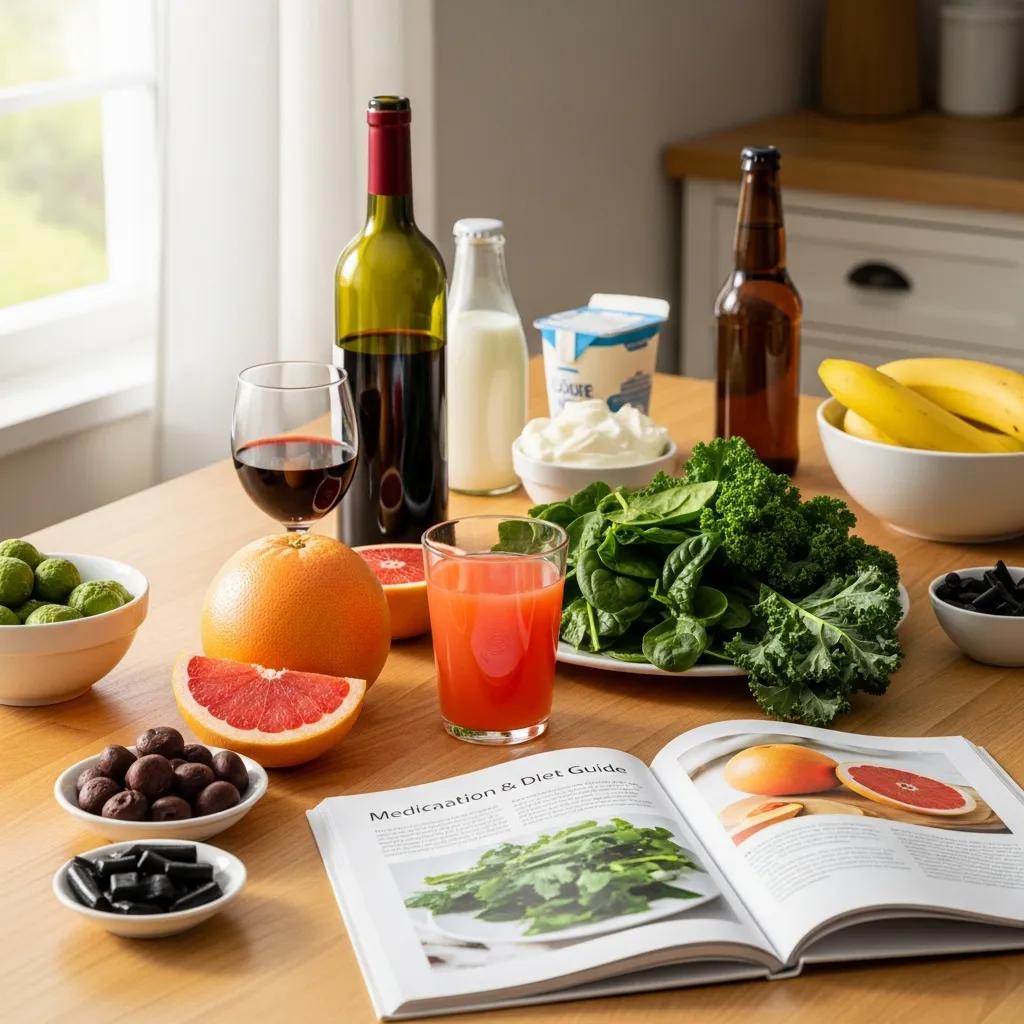
Certain foods and drinks can change medication levels quickly, but simple timing or avoidance strategies often prevent problems. For example, grapefruit juice inhibits CYP3A4 and can raise levels of some statins and other drugs, increasing the risk of toxicity. Leafy greens high in vitamin K can blunt warfarin’s effect unless intake stays consistent and INR is monitored. Alcohol can increase sedation with some medicines and raises liver risk with acetaminophen, while tyramine-rich foods can trigger dangerous blood pressure spikes with some older antidepressants (MAO inhibitors). Practical rules — avoiding grapefruit with susceptible drugs, keeping vitamin K intake steady, and skipping alcohol when taking sedatives or liver-metabolized medicines — prevent many everyday risks. Understanding these food interactions helps you compare them with the prescription and OTC risks discussed next, contributing to overall medication safety.
Before the next section, review the table below for a quick reference of interaction types, how they work, and one short real-world example each.
Introductory table: Key interaction types, how they work, and one short example for each.
| Interaction type | Mechanism | Real-world example |
|---|---|---|
| Drug-drug (pharmacokinetic) | Alters metabolism via CYP enzymes | A CYP3A4 inhibitor raises statin levels, increasing the risk of muscle damage |
| Drug-drug (pharmacodynamic) | Additive or opposing effects at the same receptors or pathways | Benzodiazepine + opioid → more sedation and higher risk of breathing suppression |
| Drug-food/drink | Food changes absorption or metabolism | Grapefruit juice inhibits CYP3A4, elevating levels of some medicines |
| Drug-condition | Disease changes drug handling or risk | Kidney failure reduces drug excretion, causing accumulation and toxicity |
Which Common Medications and Substances Cause Interactions?
Many commonly used prescription drugs, OTC medicines, and supplements have well-known interaction profiles that matter when you start, stop, or combine therapies. High-risk prescription drugs include anticoagulants, certain statins, digoxin, and medicines with narrow therapeutic windows. OTC items like NSAIDs and antacids can change bleeding risk or absorption, and herbal products such as St. John’s Wort can speed up metabolism and lower levels of many prescriptions. Knowing examples helps you decide when to ask for extra monitoring, adjust timing, or choose safer alternatives, guided by expert pharmacy advice. The next sections list typical prescription/OTC interactions and common supplement conflicts, followed by a quick-reference table with practical advice for medication safety.
What Are Typical Prescription and OTC Drug Interactions?
Interactions between prescription and OTC drugs usually stem from metabolic changes or additive side effects, and many have straightforward monitoring or avoidance strategies. For instance, warfarin’s effect can be altered by antibiotics, NSAIDs, and vitamin K–rich foods—these changes can increase bleeding risk or reduce anticoagulation, so INR monitoring and counseling are essential, according to clinical guidelines. Antacids can reduce absorption of some oral medicines, and certain antibiotics may reduce hormonal contraceptive effectiveness, so backup contraception may be recommended. OTC NSAIDs can raise blood pressure or increase bleeding risk when taken with anticoagulants. Remember: “OTC” doesn’t mean risk-free. Spotting these patterns helps you take practical steps like spacing doses, arranging temporary monitoring, or talking with a pharmacist for crucial pharmacy advice before combining medicines, thereby enhancing medication safety.
Introductory table: Common medication examples, their interacting partners, and practical advice.
| Medication | Interaction partner | Effect / practical advice |
|---|---|---|
| Warfarin | NSAIDs, antibiotics, vitamin K foods | Can increase bleeding or change INR; monitor INR and aim for consistent vitamin K intake |
| Statins (CYP3A4 substrates) | Strong CYP3A4 inhibitors or grapefruit | Raises muscle toxicity risk; avoid grapefruit and review other medicines with your pharmacist |
| Oral contraceptives | Some antibiotics, St. John’s Wort | May reduce contraceptive effectiveness; discuss backup methods when needed |
| Digoxin | Loop diuretics, certain antibiotics | Can change digoxin levels; watch for toxicity signs and monitor levels per guidance |
The cytochrome P450 (CYP) enzyme system is central to how many drugs are broken down. Understanding CYP’s role helps predict and manage interactions, a critical component of medication safety.
Understanding Cytochrome P450’s Role in Drug Interactions
Many important drug–drug interactions are explained by changes to metabolic enzymes in the liver and other tissues—especially the cytochrome P450 (CYP) family. Some drugs act as potent enzyme inducers while others are inhibitors, with inhibition reports more common in clinical practice. Knowing which drugs affect CYP enzymes is essential to safely prescribe multiple-drug regimens and to identify patients at higher risk of interactions and adverse events.
Role of cytochrome P450 in drug interactions, 2008
How Do Natural Supplements and Herbal Remedies Interact with Medications?
Natural supplements can significantly affect drug metabolism and body responses, so it’s important to tell your pharmacist about any herbs or vitamins you use. St. John’s Wort, for example, induces liver enzymes and can lower blood levels of many medications, including some contraceptives and anticoagulants. Omega‑3s or vitamin E can affect clotting when taken with anticoagulants, raising bleeding risk. People often assume supplements are harmless, but they can change how drugs work or worsen medical conditions. Always list supplements on your medication record and ask your pharmacist for expert pharmacy advice about conflicts before starting new herbal products. This makes unexpected interactions less likely and sets you up to use the prevention steps described next—like keeping one pharmacy for centralized review, a key strategy for medication safety.
The inhibition or induction of CYP enzymes by drugs, supplements, and herbal remedies is a primary mechanism behind many pharmacokinetic interactions, as highlighted by medical research.
CYP Enzyme Inhibition and Induction: Mechanisms of Drug Interactions
The cytochrome P450 (CYP) family is a key enzyme system for phase I metabolism of drugs and other compounds, including herbal remedies. Inhibition or induction of specific CYP enzymes is a major cause of pharmacokinetic drug–drug interactions. This review updates inhibitors and inducers of human CYP enzymes, summarizes recent in vitro and in vivo findings, and discusses clinically relevant examples such as tyrosine-kinase inhibitors and antiretroviral HIV medications.
Inhibition and induction of CYP enzymes in humans: an update, J Hakkola, 2020
How Can You Prevent Drug Interactions and Ensure Medication Safety?

Preventing interactions comes down to good documentation, clear communication, and a few simple habits that cut risk for most patients—especially those on many medicines. Key steps include keeping an up-to-date medication list (prescription, OTC, and supplements), using one pharmacy for prescriptions, reviewing medications regularly with a pharmacist, and reading labels or asking for counseling when you start a new medicine. These habits close information gaps that lead to missed interactions and let pharmacy systems flag problems early, significantly improving medication safety. Below are concrete prevention steps you can add to your routine, based on expert pharmacy advice.
- Keep an updated medication list that includes prescriptions, over‑the‑counter products, and supplements.
- Use one pharmacy for fills and refills so pharmacists can review your complete profile.
- Schedule regular medication reviews—especially after hospital stays, new diagnoses, or when several new medicines are started.
- Read labels and ask a pharmacist about food, drink, or supplement restrictions whenever you start a new medicine.
These simple actions create a routine that lowers interaction risk and gets you ready for pharmacist-led reviews described next, reinforcing your commitment to medication safety.
Introductory table: Actions, who benefits most, and how to implement each prevention step.
| Action | Who it helps | How to do it |
|---|---|---|
| Keep updated med list | Anyone on medication, especially older adults | Carry a printed or digital list and update it after every change |
| Use one pharmacy | People with multiple prescribers or on many medicines | Consolidate prescriptions at a single pharmacy to enable full profile checks |
| Schedule medication reviews | Patients on anticoagulants, multiple meds, or new therapies | Book a pharmacist review after medication changes or hospital discharge |
| Read labels and ask questions | All patients | Check label warnings and consult your pharmacist before mixing with alcohol or supplements |
These practical entries put prevention into clear steps you can follow and make pharmacy services more useful for managing drug interactions.
Value Drugstore can help put these steps into practice with pharmacist medication reviews and telehealth follow-ups that reinforce the checklist above. As a community-focused e-commerce and information hub serving the Belvedere Square area, Value Drugstore emphasizes personalized care: our pharmacists review your full medication profile, reconcile prescriptions and supplements, and offer telehealth consultations for follow-up questions. Consolidating refills with one pharmacy improves medication safety because pharmacy software flags known interactions and pharmacists can coordinate with prescribers when adjustments are needed. That close alignment between patient habits and pharmacy workflows makes everyday prevention steps easier to follow, providing invaluable pharmacy advice.
When Should You Consult Your Pharmacist About Drug Interactions?
Contact a pharmacist whenever you add a new prescription, OTC product, or supplement, or if you notice unexplained symptoms that could signal a drug interaction. Pharmacists can quickly assess risk, recommend monitoring or safer alternatives, and coordinate with prescribers, offering essential pharmacy advice. Other clear triggers for a pharmacist review include having multiple prescribers, a recent hospital discharge, or a new diagnosis that affects drug handling (like kidney or liver disease). Pharmacists can triage urgency, suggest immediate precautions, and help avoid both under- and over-reactions to possible interactions, ensuring your medication safety. Below are common warning signs and a description of how telehealth reviews can help.
- Unexplained bleeding, bruising, or dark stools — signs that anticoagulation may be too strong.
- Severe drowsiness, confusion, or trouble breathing after starting or increasing sedatives.
- Rapid heartbeat, fainting, or sudden blood pressure swings after a medication change.
- New stomach symptoms, muscle pain, or jaundice that could signal organ toxicity.
These warning signs point to next steps: stop a nonessential suspect medicine if symptoms are severe and seek emergency care, or contact a pharmacist promptly for advice on monitoring and dose changes, prioritizing your medication safety.
What Signs Indicate a Possible Drug Interaction?
Signs range from mild to serious. Mild symptoms include new stomach upset, lightheadedness, or extra tiredness after starting a medicine. More serious signs include unusual bleeding, severe drowsiness, chest pain, or marked blood pressure changes that need urgent attention. If worrying symptoms start soon after a medication change, stop any nonessential OTC or supplement and contact your pharmacist or prescriber right away for immediate pharmacy advice. Pharmacists can recommend immediate precautions and tell you whether emergency care is needed. Keeping a medication timeline — noting when you started each drug and when symptoms began — helps the pharmacist determine the likely cause and next steps, crucial for managing drug interactions.
How Can Telehealth Consultations Support Medication Reviews?
Telehealth medication reviews give you fast access to a pharmacist when you can’t visit in person. They work well for reviewing medication lists, spotting interactions, and arranging follow‑up monitoring. Before a telehealth review, prepare a full medication list, note recent changes, and write down questions about side effects or food interactions. The pharmacist will review your profile, flag any concerns, and recommend labs or prescriber contact if needed, providing personalized pharmacy advice. Telehealth is useful after hospital discharge, for older adults on many medicines, or when extra counseling is needed after starting a new therapy. Combining telehealth with in-store services keeps your records current and reduces interaction risk, enhancing overall medication safety.
Value Drugstore offers both telehealth consultations and in-store medication reviews so you can get timely pharmacist advice on potential interactions in the way that suits you best.
How Does Value Drugstore Support You in Managing Drug Interactions?
Value Drugstore helps keep you safe by combining pharmacy software with pharmacist-led reviews, compounding services, and easy telehealth access to spot and prevent drug interactions. As an e-commerce and local information hub in the Belvedere Square community, Value Drugstore provides prescription refills, personalized compounding when standard products aren’t right, immunizations, a selection of supplements, and telehealth consultations to connect you with a pharmacist for medication reviews. Our pharmacists use a complete medication profile to flag drug–drug, drug–food, and supplement interactions and to counsel patients on monitoring, timing, and lifestyle changes that lower risk. The service model prioritizes patient education and coordinated care—encouraging prescription consolidation and routine follow-up to keep your medication record up to date, all contributing to superior medication safety and expert pharmacy advice.
- Medication reconciliation and profile maintenance to centralize prescriptions and supplements.
- Pharmacist medication reviews via telehealth and in-person counseling to assess interactions and monitoring needs.
- Personalized compounding to avoid problematic ingredients or tailor dosing when commercial products don’t fit.
These services help patients with complex regimens by offering clear, actionable plans—such as dose adjustments, monitoring schedules, or safer alternatives—that reduce interaction risk while preserving treatment benefits, a testament to our commitment to medication safety.
What Pharmacy Services Help Identify and Prevent Interactions?
Key pharmacy services that identify and prevent drug interactions include medication reconciliation, computerized interaction checks, scheduled medication reviews, and compounding to modify formulations for safety. Medication reconciliation collects prescriptions, OTCs, and supplements into one profile so interaction checks can detect risky combinations and prompt pharmacist counseling. Telehealth medication reviews and in-store consultations let pharmacists explain risks, recommend lab monitoring, and coordinate with prescribers to change therapy when appropriate. Compounding can remove problematic excipients or provide alternative dosing for patients with allergies or special needs. These coordinated services create a safety net that’s especially valuable for people with polypharmacy or chronic conditions, ensuring comprehensive medication safety and reliable pharmacy advice.
How Do Pharmacists Provide Personalized Medication Interaction Advice?
Pharmacists follow a clear process: collect a complete medication list, assess interaction risk with clinical knowledge and checking tools, counsel patients on monitoring or alternatives, and document follow-up actions for continuity of care. A typical consult may lead to recommendations like spacing doses to avoid absorption problems, changing therapy to reduce additive effects, ordering lab monitoring, or contacting a prescriber to adjust drugs. Pharmacists also give practical lifestyle advice—such as keeping vitamin K intake steady on warfarin or avoiding grapefruit with certain statins—to lower everyday risk. This personalized approach blends evidence-based checks with patient-centered counseling and follow-up to keep medication use safe over time, providing expert pharmacy advice for optimal medication safety.
Frequently Asked Questions
What should I do if I suspect a drug interaction?
If you think a drug interaction may be happening, stop any non-essential OTCs or supplements that could be involved and monitor your symptoms. Contact your pharmacist or healthcare provider right away — they can review your medications, advise on monitoring, and suggest safer alternatives if needed. Having a complete list of all medicines and supplements will help them give accurate guidance and expert pharmacy advice. Acting promptly can prevent complications, so don’t hesitate to reach out for help to ensure your medication safety.
How can I safely manage multiple medications?
Managing multiple medications well takes organization and communication. Keep an up-to-date medication list that includes prescriptions, OTCs, and supplements. Use a single pharmacy for fills so pharmacists can check your full profile. Arrange regular medication reviews with your pharmacist, especially after health changes or new prescriptions, to get personalized pharmacy advice. This proactive routine helps keep your treatment effective while reducing the risk of harmful interactions and enhancing medication safety.
Are there specific populations at higher risk for drug interactions?
Yes. Older adults often take more medicines for chronic conditions and are at higher risk for drug interactions. People with liver or kidney disease may handle drugs differently and also face higher risk. Anyone using herbal supplements or multiple OTC products without checking with a clinician can increase their chance of an interaction. Awareness of these factors helps guide preventive steps and targeted monitoring, crucial for medication safety.
What role do pharmacists play in preventing drug interactions?
Pharmacists are central to preventing drug interactions: they review medication lists, spot potential conflicts, and provide personalized counseling. They assess interaction risk based on your full medication and health history and advise on monitoring, timing, or alternative treatments. By offering medication reviews and education, pharmacists help ensure medications are used safely and effectively, providing invaluable pharmacy advice for optimal medication safety.
How can I prepare for a telehealth medication review?
Before a telehealth review, gather a complete list of all medicines — prescriptions, OTCs, vitamins, and supplements — and note recent changes or new symptoms. Write down questions about side effects, food interactions, or dosing. Be ready to describe how you take each medicine. This preparation helps the pharmacist do a thorough review and give tailored pharmacy advice to improve your medication safety.
What are the signs of a serious drug interaction?
Signs of a serious drug interaction include unexplained bleeding or bruising, severe drowsiness, confusion, trouble breathing, persistent nausea or vomiting, rapid heartbeat, fainting, or sudden large changes in blood pressure. If any of these occur after starting or changing a medication, seek immediate medical attention. Early recognition and intervention can prevent serious harm and are vital for medication safety.
What Are the 3 Main Types of Drug Interactions?
The three main types are drug-drug, drug-food/drink, and drug-condition interactions. Drug-drug interactions usually involve changes in metabolism or additive effects and can increase toxicity or reduce benefit. Drug-food/drink interactions happen when foods or beverages change absorption or metabolism. Drug-condition interactions occur when an underlying disease alters drug handling or safety. For example, warfarin can be affected by antibiotics (drug-drug), by large changes in vitamin K intake (drug-food), or by liver disease that changes metabolism (drug-condition). Identifying the type helps you pick the right response—monitoring, dose adjustment, or avoiding the combination—a key part of ensuring medication safety.
Which Foods Should Be Avoided with Certain Medications?
Some foods and drinks commonly interact with medicines, so practical avoidance or consistent intake is often recommended, based on expert pharmacy advice. Avoid grapefruit with drugs metabolized by CYP3A4 (including some statins), keep vitamin K intake steady if you take warfarin, avoid alcohol with sedatives or acetaminophen, and skip tyramine-rich foods if you use certain older antidepressants (MAO inhibitors). When in doubt, ask your pharmacist. These simple rules reduce preventable interaction risks and work alongside medication checks and pharmacist counseling described earlier, contributing significantly to medication safety.
- Grapefruit: avoid with CYP3A4 substrates such as some statins.
- Leafy greens (vitamin K): keep intake consistent while on warfarin therapy.
- Alcohol: avoid with sedatives, certain pain relievers, and drugs processed by the liver.
These short cautions give immediate guidance and point you to pharmacist review for more personalized pharmacy advice.
Conclusion
Knowing how drug interactions happen and taking a few practical steps can make medication safety much stronger. Recognize the main interaction types, keep an updated medication list, and consult your pharmacist regularly for expert pharmacy advice. Simple prevention strategies—paired with pharmacist support and telehealth reviews—can greatly reduce the risk of adverse effects. For personalized medication safety and expert pharmacy advice, always consult with a qualified healthcare provider or your Value Drugstore pharmacist. Your health is our priority. Take control of your medications today by using our pharmacy services for personalized medication management and safety.



